POWER OF PLUS WITH
PURAPLY®AM & PURAPLY®XT
Native matrix scaffold + broad-spectrum PHMB antimicrobial for next-level wound healing
A native, cross-linked extracellular matrix scaffold + sustained antimicrobial effectiveness within the product to support wound healing and aid in granulation tissue formation.
NEW STANDARD OF CARE
Take control before biofilm re-forms. Bioburden management with PuraPly®AM and PuraPly®XT helps you move wounds out of the inflammatory phase.
- Native ECM structure provides a scaffold for cellular migration and proliferation
- Provides sustained antimicrobial effectiveness within the product between patient visits5,6
- Provides a proactive foundation of care for controlling bioburden and preventing biofilm re-formation†2-4
THE POWER OF PLUS
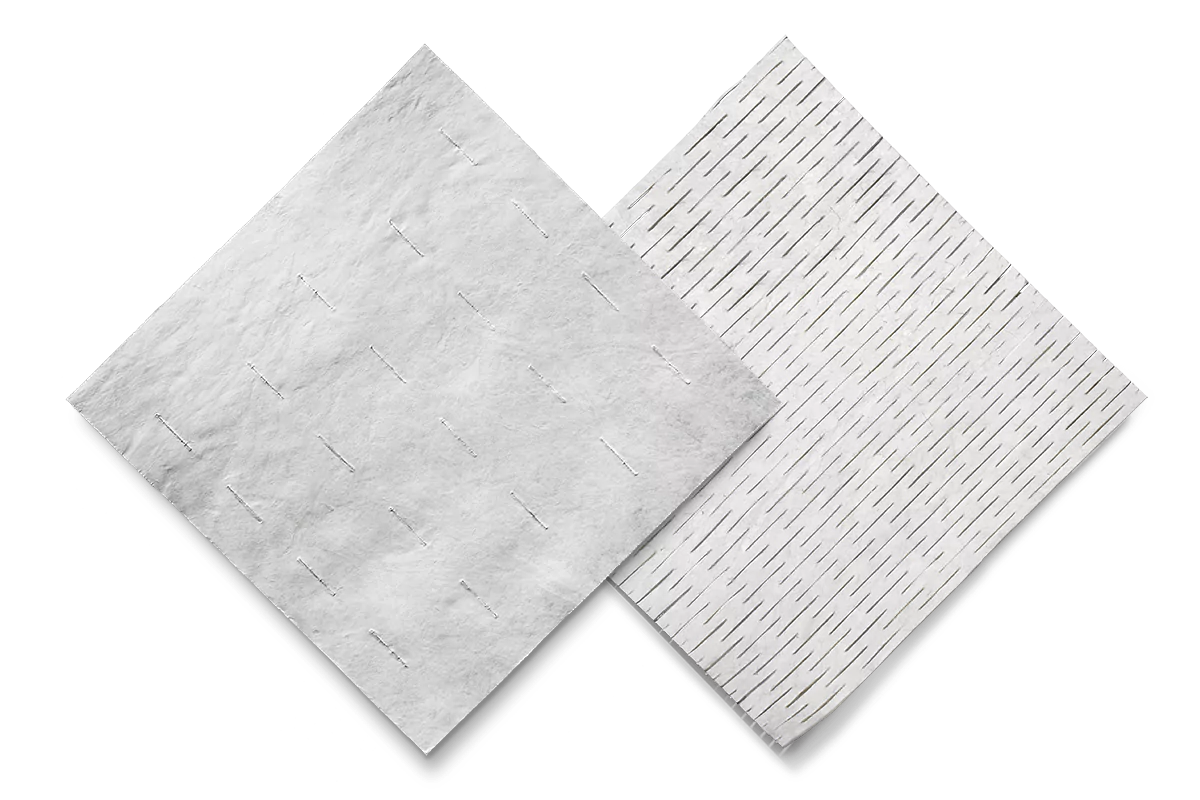
Only PuraPly®AM and PuraPly®XT combine a native ECM scaffold + broad-spectrum PHMB antimicrobial for next-level wound healing support
THE POWER OF PLUS
NATIVE, CROSS-LINKED ECM
Provides a scaffold for cellular
migration and proliferation
![]()
BROAD-SPECTRUM PHMB
Helps control bioburden2-5
ECM=extracellular matrix;
PHMB=polyhexamethylene biguanide
THE POWER OF PLUS: INDEPENDENTLY UNIQUE, COLLECTIVELY IN CONTROL
NATIVE, CROSS-LINKED ECM SCAFFOLD
Supports wound healing and aids in granulation tissue formation
- Native ECM structure provides a scaffold for cellular migration and proliferation
- Native ECM scaffold inhibits a wider range of MMPs, helping to address the proinflammatory proteolytic environment that stalls wounds9
- The cross-linked, dual layers of PuraPly AM and five layers of PuraPly XT resist ECM scaffold degradation in the wound, supporting persistence between patient treatments3,8
- The native ECM scaffold fibers of PuraPly®AM and PuraPly®XT have been uniquely strengthened with EDC to increase the number of molecular bonds, which improves their resistance to protease degradation9-11
- The dual layers of PuraPly AM and five layers of PuraPly XT maximize surface area for PHMB saturation1,3,8
Proprietary purification process
- Preserves the natural extracellular matrix scaffold structure to ensure strength, function, and biocompatibility during wound healing
- Removes cells and non-collagen materials that could cause an inflammatory/immunologic response
- Inactivates viruses and bacteria
BROAD-SPECTRUM PHMB
Proactively disrupts bioburden1,3,4
Unlike silver dressings, PHMB:
- Does not damage key cells (eg, fibroblasts) involved in wound healing5,12
- Features high tissue compatibility and low cytotoxicity2,4,5,13
- Has no known instances of bacteria acquiring resistance2-4,14
- Provides a persistent antimicrobial effect within PuraPly®AM and PuraPly®XT1,5
EDC=l-Ethyl-3-(3-dimethylaminopropyl)carbodiimide
PERSPECTIVE PAPER SERIES
Specialists, nurses, and researchers across the wound care space provide their perspectives on the impact of biofilm and the importance of biofilm management.

Gregory Schultz, PhD A comprehensive biofilm-based management approach: improving standard of care for all wound types.
DOWNLOAD PAPER

John H. Samies, MD, FSHEA, CWSMarie L. Gehling, MSN, NP-C, CWOCNPuraPly AM for a comprehensive biofilm-based wound management approach.
DOWNLOAD PAPERCONFIRMATION OF CONTROL
See more product details from PuraPly AM and PuraPly XT, or contact an Organogenesis Tissue Regeneration Specialist to see how PuraPly AM and PuraPly XT can help your practice.
Please refer to the PuraPly AM Instructions for Use and PuraPly XT Instructions for Use for complete prescribing information.
REFERENCES:
- PuraPly Antimicrobial [package insert]. Canton, MA: Organogenesis Inc; 2020.
- Hübner NO, et al. Skin Pharmacol Physiol. 2010;23(1 suppl):17-27.
- Brantley J, et al. Wounds Int. 2016;7(3):1-5.
- Gilbert P, et al. J Appl Microbiol. 2005;99(4):703-715.
- Davis SC, et al. Int Wound J. 2021. Epub ahead of print. doi:10.1111/iwj.13600
- Data on file. PDR-0001. Organogenesis Inc.
- Wolcott RD, et al. J Wound Care. 2010;19(8):320-328.
- Carpenter S, et al. Wounds. 2016;28(6 suppl):S1-S20.
- Negron I, et al. Int Wound J. 2014;11(4):392-397.
- Khor E. Biomaterials. 1997;18(2):95-105.
- Billiar K, et al. J Biomed Mater Res. 2001;56(1):101-108.
- Zou SB, et al. Int Wound J. 2013;10(3):306-312.
- Sood A, et al. Adv Wound Care. 2014;3(8):511-529.
- Sim W, et al. Antibiotics. 2018;7(4):93.